KEY TO A NEW VISUAL START FOR YOUR PETS
What are Cataracts?
The lens inside an eye is analogous to a peanut M&M. The outside of the lens is called the “capsule” and is similar to the candy shell coating on an M&M. The “cortex” of the lens is like the chocolate part of the M&M and the “nucleus” would be the peanut. Functionally, the lens is similar to the lens of a camera and allows the eye to focus properly.
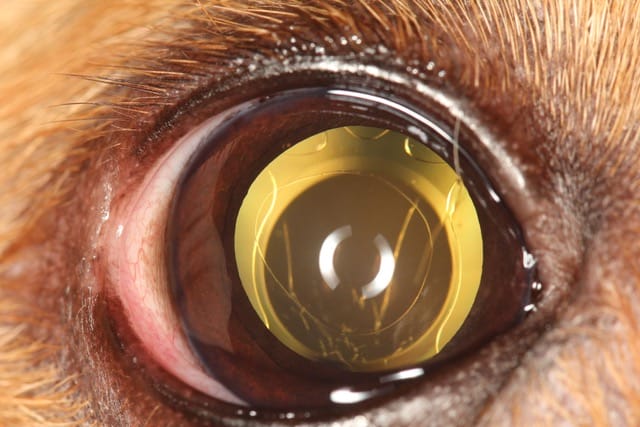
A cataract is a condition when the normally clear lens becomes cloudy. To use another food analogy, think about an egg white. When you crack an egg, the egg whites are clear enough to read a paper through. However, when you cook the egg whites, they go from clear to opaque. This is similar to what happens when a cataract forms. The normally clear lens becomes opaque or cloudy.
Cataracts can range in size, from a small dot in the lens to involving the entire lens. When a cataract forms, it results in decreased vision. Initially the decrease can be mild and similar to having dirty glasses or low vision on a foggy day. In the early stages it may not noticeably affect your pet’s vision. When the cataract is mature or complete, all functional vision is lost, and it is similar to looking through several sheets of wax paper. At this advanced stage, you will notice your pet bumping into furniture and walls.
The most common sign of cataracts is a white color change or cloudiness within the eye. You may notice a diminishment in vision or even a complete vision loss depending on how developed the cataract may be. Additionally, your pet may experience pain/discomfort due to inflammation caused by the cataracts. Symptoms associated with ocular pain include squinting, excessive tearing, increased redness or swelling of the eye.
In dogs, the most common cause of cataract formation is genetics. The cataracts are inherited and can either be present at birth (congenital) or can develop later in life. The second most common cause of cataracts in dogs is diabetes mellitus. Diabetic cataracts tend to develop very quickly. Statistics show that 80% of dogs with diabetes will develop complete cataracts within 1 year of developing diabetes. Other causes of cataract formation include trauma, intraocular inflammation (uveitis), and nutrition. In cats, cataracts are typically not genetic but form secondary to trauma or uveitis.
Cataracts are diagnosed by completing a thorough eye exam on your pet similar to the eye exam performed by your own eye doctor. This exam will help us to establish whether your pet’s vision can be improved through cataract surgery as well as look for any other problems or diseases of the eye. A series of diagnostic tests will be performed during your pet’s initial exam and will include: tear production measurement, measuring the intraocular pressure (IOP) of the eye, and staining to evaluate the ocular surface.
Treatment of your pet’s cataracts will depend on the stage and cause of the cataract, as well as any other eye problems that may be found during the initial exam. The only effective treatment for advanced cataracts is surgical removal. If the cataract is small and vision is not impaired, we may recommend periodic monitoring through follow up visits to determine progression of the cataracts. Some cataracts do not change and may not require surgery.
If you elect not to have cataract surgery, your pet may need to be placed on daily topical drops to control the inflammation caused by the cataracts.
If advanced cataracts are left untreated, over time they can luxate, or become loose from the structures that hold them in place. This allows the cataract to shift positions within the eye where it can block the normal fluid flow leading to glaucoma. Glaucoma is a painful and blinding disease that often leads to eye removal.
It is necessary to ensure that your pet has a healthy retina prior to cataract surgery. The retina is a tissue paper-like membrane in the back of the eye that allows for vision, analogous to the film in a camera. If the retina is not functioning properly, removing the cataract and implanting an artificial lens will not improve your pet’s vision. We perform two tests to evaluate retinal function prior to cataract surgery; an electroretinogram (ERG) and an ocular ultrasound (US). The ERG is similar to that of an EKG for your heart. It tests the electrical activity or function of the retina. The ultrasound allows us to evaluate the structure of the eye by giving us visualization of the posterior segment.
The ERG requires that we “dark adapt” your pet’s eyes. We will place them in a dark exam room for 20-30 minutes prior to performing the test. These tests are not painful and can be done on most pets without any sedation. Both tests will take around an hour for completion.
Cataract surgery in pets is very similar to cataract surgery in people and is the only way to restore vision following cataract formation. Under general anesthesia, a small incision is made into the eye. An ultrasonic hand piece (similar in size to a large ink pen) is used to break up the cataract and aspirate it out of the eye. Then an artificial lens is inserted to restore your pets normal refraction. After removal of the cataracts, your pet will not develop cataracts again.
The surgery is performed on an OUTPATIENT basis meaning your pet will go home the same day the surgery is performed. This surgery is approximately 95% successful however, the results can be variable based on individual cases initial findings. With a successful surgery most patients regain near normal vision, although most are slightly far sighted. As a result, their vision is slightly out of focus when viewing objects at a close distance (a few feet). Most pets experience improved vision immediately and vision typically continues to improve over the 3 to 7 days following surgery.
While successful in the majority of patients, there are risks associated with the procedure. Complications associated with cataract surgery include:
- Inflammation (uveitis) – Inflammation associated with cataracts must be treated whether surgery is pursued or not. Cataract formation in dogs induces an allergy like immune response to the cataract that will need to be treated, typically with life long therapy.
- Glaucoma – Glaucoma is a disease associated with increased intraocular pressure. 20% of patients with cataracts will go on to develop glaucoma. If surgery is performed we can typically reduce this to about 5% however, glaucoma can still be a cause of vision loss following cataract surgery.
- Retinal Detachment – This is an infrequent complication of cataract surgery but can be a cause of vision loss following the procedure.
- Infection – This is a risk associated with any surgery however it is rarely seen with this procedure.
- Trauma – Unfortunately we cannot tell our pets not to rub their eyes after surgery, therefore, we send them home wearing a medical collar for 1-2 weeks to prevent any damage to the surgery site.
Post-operative care involves eye drops as well as oral medications. The first 2 weeks involves multiple eye drops 4 times a day which is typically reduced to once a day long term therapy by the two month recheck. The first post-op appointment will be required the morning after your pet’s surgery. We then recheck at one week, two weeks, 1 month, and 2 months after surgery. Periodic follow up examinations are then scheduled on a 6 month to a yearly basis to ensure your pet remains pain free and visual for life.